Last Updated on January 31, 2022 9:21 am
(Raleigh, N.C.) – North Carolina’s nonprofit hospitals are billing poor patients at an average rate up to three times the national average. State Treasurer Dale R. Folwell, C.P.A., Rep. Edward Goodwin, Rep. Howard Hunter, Sen. Jay Chaudhuri and Sen. Jim Burgin called on lawmakers to increase accountability and protect patients during a press conference Wednesday, Jan. 26.
Treasurer Folwell invited National Academy of State Health Policy researchers to extend their national analysis of hospitals to North Carolina. Together with the North Carolina State Health Plan, these researchers found that failures in charity care exposed poor patients to bills and medical debt. The study was peer reviewed by Dr. Vivian Ho, James A. Baker Institute Chair in Health Economics at Rice University.
Some of North Carolina’s nonprofit hospitals have billed $149.2 million to poor patients who should have qualified for free or discounted charity care under the hospitals’ own policies in fiscal year 2019. This is an underestimate that accounts for only one in six hospitals in the state.
“Failures in charity care have real consequences for real patients – especially those with low or fixed incomes, who should be protected instead of punished,” Treasurer Folwell said. “Only one in five hospitals’ charity care justified their tax breaks. Instead, some hospitals sent out bills to the most vulnerable residents of our state. These patients can’t afford these bills — and most couldn’t even find out what their bill was until it was too late.”
When patients don’t receive charity care, hospitals attempt to collect their bills, sometimes by damaging credit scores, garnishing wages, suing patients or encouraging them to open a medical credit cards than can charge interest. If a hospital gives up on collecting a bill, the hospital absorbs the cost and writes it off as bad debt. Charity care is meant to protect patients from this process, but the Internal Revenue Service does not set a threshold for charity care spending or eligibility.
In North Carolina, up to 28.7% of hospital bad debt was billed to impoverished patients likely eligible for charity care in fiscal year 2019. The report’s findings also point to a possible, disturbing spike in billing poor patients instead of providing charity care during the pandemic. Consumer debt is on the rise, while some of the largest hospitals recorded rising profits during the pandemic.
“When we tried to make health care more affordable for teachers, state and local employees and their families, hospitals justified overcharging patients and taxpayers by pointing to charity care,” said Treasurer Folwell. “We need to hold these multimillion-dollar executives and their multibillion-dollar nonprofits accountable for how they treat the invisible men and women of North Carolina.”
“North Carolina’s analysis of available data on bad debt paid as part of hospitals’ community benefit expenditures helps increase health cost transparency,” said Bartlett. “Like North Carolina, an increasing number of states are seeking to better understand hospital costs, including community benefit expenditures with the goal of driving these investments towards meaningfully supporting the community’s health.”
“Nonprofit hospitals are shielded from taxes with the expectation that they will direct their resources toward local community benefit,” said Ho. “I am disturbed by how many North Carolina nonprofits are abusing that privilege to boost their profits at the expense of average citizens struggling to make a living.”
Key findings:
In North Carolina nonprofit hospitals face very little accountability for their charity care and bad debt.
- Neither the federal nor the state government fully require a minimum threshold for community benefit spending or charity care eligibility.
- Worse, the Internal Revenue Service cannot demonstrate that it is consistently reviewing hospitals’ community benefits.
Some North Carolina nonprofit hospitals are billing poor patients instead of providing charity care, despite receiving more than $1.8 billion in tax breaks.
- North Carolina nonprofit hospitals should have provided an average 11.9% to 28.7% of their bad debt as charity care in FY 2019 — a rate up to almost three times the national average of 10%.
- When patients don’t qualify for charity care, hospitals attempt to collect on bills, sometimes through damaging credit scores, suing patients, or encouraging them to open medical credit cards that charge interest. If a hospital gives up, the bill becomes bad debt.
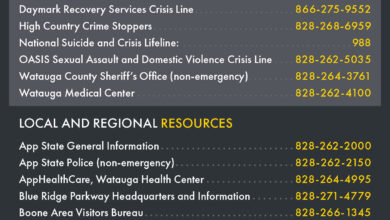
- Atrium Health Wake Forest Baptist, UNC Health, Cone Health, and AccessOne Health encouraged patients to use medical credit cards that can charge interest rates as high as 18% after a promotional period.
Eighteen nonprofit hospitals billed almost $150 million to poor patients who should have qualified for charity care under the hospitals’ own policies.
- This is an underestimate because only 16% of North Carolina hospitals provided reliable data, and many do not have to publish any data at all.
The pandemic is expected to intensify the problem.
- One in five North Carolina families had medical debt in collections in 2020, according to the Urban Institute.
- The levels of bad debt eligible for charity care were worse in 2020 than in the previous fiscal year. Nonprofit hospitals estimated that an average 31% to 48% of their bad debt should have been charity care in fiscal year 2020, according to the little data available.
Without standards and accountability, it has become difficult to tell nonprofit hospitals apart from for-profits.
- Only one in five nonprofit hospitals provided enough charity care to equal the value of their tax exemptions in FY 2019.
- On average, North Carolina’s hospitals were three times more profitable than the national average operating profit margin. But these profits are not trickling down to patients.
- Some nonprofit hospitals even billed more than 60% — and 80% — of their bad debt to disadvantaged patients likely eligible for charity care.
We need accountability and transparency.
- There is precedent for states to strengthen accountability. Other states require profitable hospitals to justify their tax exemptions with community benefits.
- Utah, Illinois, Oregon and Nevada all require a minimum threshold for community benefit spending. Pennsylvania instituted defined standards and California mandated a more generous eligibility policy for charity care.
- North Carolina should follow other states’ example in requiring thresholds for profitable nonprofit hospitals’ community benefits.
See Report: North Carolina Nonprofit Hospitals Bill the Poor.